
Steps to Overcoming Teenage Anger
Seriously, It’s time to end mental health stigma because seeking support is healthy. As a licensed mental health therapist, I often meet folks new to therapy afraid and embarrassed to connect to mental health support….and why? Because of the stigma of connecting to mental health stigmas:
I don’t want to look weak.
Does this mean I’m crazy?
Going to therapy means something is really, really wrong.
What will my family think of me?…my friends?
Going to therapy means I lost faith in God.
I’m a failure.
People do have good reasons to have these thoughts. Media and movies do not do a good job at accurately depicting what a person living with mental health issues commonly looks like. Most movies show a white person living with a severe mental diagnosis, characters like The Joker.
Go to the mirror, that is what a person living with a mental health need can look like. Mental health issues are not always witnessed or visible; and mental health needs run on a spectrum. A person struggling with depression or anxiety can look like a very happy person that cracks a lot of jokes. A person struggling with anxiety can look like a moody loved one that always cancels last minute events, a successful executive that spends more time in the office than with family and friends, or a physically fit person that does yoga that excessively counts calories, and weights themselves.
Every person on this Earth will experience depression or anxiety at some point in their lives. Yes, including me and you. It is very human to feel sad when you see, hear, or experience sad things: like a loss of a job, disappointment in a dream deferred, or being physically hurt. It is also very human to experience feeling on edge and restless during uncertainty ( i.e.., coping with this pandemic or being a BIPOC male pulled over by the police). Not all symptoms warrant a mental health diagnosis, but every person can benefit from mental health support. Honestly, most people are having a very normal reaction to abnormal circumstances. Your emotional self is directly connected to your physical self. Unaddressed mental health needs can cause issues in other parts of our lives.
It is no wonder that depression is a leading cause of disability worldwide and is a major contributor to the overall global burden of disease.

Facts:
Number of African Americans with Mental Illness: 6.8 million
- Black and African American people living below poverty are twice as likely to report serious psychological distress than those living over 2x the poverty level.
- Adult Blacks and African Americans are more likely to have feelings of sadness, hopelessness, and worthlessness than adult whites.
Number of Latinx/Hispanic Americans with Mental Illness: 8.9 million
- Religion can be a protective factor for mental health in Latinx/Hispanic communities (faith, prayer) but can also contribute to the stigma against mental illness and treatment (demons, lack of faith, sinful behavior), so targeting religious institutions to help encourage good mental health and treatment-seeking is important.
- There is a perception in Latinx/Hispanic communities, especially among older people, that discussing problems with mental health can create embarrassment and shame for the family, resulting in fewer people seeking treatment.
Number of Asian Americans with Mental Illness: 2.2 million
- Serious mental illness (SMI) rose from 2.9 percent (47,000) to 5.6 percent (136,000) in AAPI people ages 18-25 between 2008 and 2018.
- Major depressive episodes increased from 10 percent-13.6 percent in AAPI youth ages 12-17, 8.9 percent to 10.1 percent in young adults 18-25, and 3.2 percent to 5 percent in the 26-49 age range between 2015 and 2018.
- Suicidal thoughts, plans, and attempts are also rising among AAPI young adults.
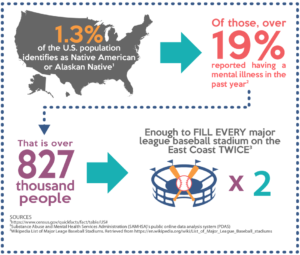
Number of Native Americans/Alaskan Natives with Mental Illness: 830,000
- Native/Indigenous people in America report experiencing serious psychological distress 2.5 times more than the general population over a month’s time.
- Although overall suicide rates are similar to those of whites, there are significant differences among certain age groups. The suicide death rate for Native/Indigenous people in America between the ages of 15-19 is more than double that of non-Hispanic whites.
- Native/Indigenous people in America start to use and abuse alcohol and other drugs at younger ages, and at higher rates, than all other ethnic groups.
The Kaiser Foundation conducted a longitudinal study that found that social factors were the greatest determinant of health. These Social determinants of health (SDOH) are the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks. The unique lived experiences of BIPOC also highlight treatment barrier for BIPOC connecting to adequate support like access to culturally humble providers or providers that speaking the respective languages.There are specific stressors faced by BIPOC that can contribute to overwhelming emotional overwhelm: targeted police brutality, hate crimes, immigration family separation, and the day-to-day persistent experience of microaggression in predominantly white spaces like education or the workplace.Needless to say, Black, Indigenous, People of Color can benefit from safe spaces to explore mental health support.
We are de-stigmatizing mental illness and seeking support by having the important conversation. We are normalizing having difficult but important conversations about our health and mental health needs.

Here is what you can do:
1. Honest conversations
Check-in with yourself. Schedule weekly or monthly check-ins with yourself about how you are doing emotionally and physically. Ask, yourself what do I need more of and less of? Make a list of these two, and then write down the barriers to achieving it.
2. Ask for help / Tell PCP
Now that you have made a list. Ask yourself, do you have someone in your life that you are willing to ask? The worst thing they can say is no, but at least you give others an opportunity to help if they are available to help.
It is always a great practice to call or message your Primary Care Provider (PCP) about feeling depressed or anxious. Your PCP can help you explore options for care.
3. Research ahead of time for self & others
Explore options for care on your own. Depending on your community, there may be others you can connect with or resources available. Sometimes, family or friends will come to you for help and you may be lost on how to support. Save numbers like a Medical Adviceline or local Suicide hotline to your phone to keep handy. (Here’s a head start, Suicide prevention : 800-273-8255)
4. Develop a Care Routine
Everyone has their own unique ways that they take care of their emotional selves. Some benefit from spending time in nature, being with animals, exercising or prayer. Whether it is taking naps or connecting with family and friends. Last year, weekly therapy and Bible Study helped me. This year, I’m monitoring my blood pressure and practicing in group exercise to care for myself .Explore and learn new ways to replenish, recharge, and care for yourself.
5. Connect to Professional, Licensed Therapist
That is what they do! Licensed Psychotherapist can be LMFT, LCSW, PhD, Psy.D or Psychiatrist. These mental health professionals are trained to diagnose and treat mental health issues. Some providers specialize in specific issues or certified and trained to administered certify types of therapeutic modalities (i.e.., EMDR, Brainspotting, hypnosis, etc.).
6. Medication
Yup medication, I have to say it. Some people benefit from medication management of symptoms due to hormonal imbalances or when psychotherapy has not been helpful enough. It is your body, you make the choice. Many people have received emotional relief and regained balance from psychotropic medications. Again, always consult with your medical provider or therapist.

- Eating or sleeping too much or too little
- Pulling away from people and usual activities
- Having low or no energy
- Feeling numb or like nothing matters
- Having unexplained aches and pains
- Feeling helpless or hopeless
- Smoking, drinking, or using drugs more than usual
- Feeling unusually confused, forgetful, on edge, angry, upset, worried, or scared
- Yelling or fighting with family and friends
- Experiencing severe mood swings that cause problems in relationships
- Having persistent thoughts and memories you can’t get out of your head
- Hearing voices or believing things that are not true
- Thinking of harming yourself or others
- Inability to perform daily tasks like taking care of your kids or getting to work or school
We can help connect you with a therapist at Urban Catalyst Psychotherapy:
https://www.urban-catalyst.org/
Join our Wellness Programs and Series:
-Stay up-to-date by visiting our Events page
https://www.urbanhealthgroupllc.com/events.html
-Life / Work Balance Reset Series
-Couples Communication SeriesWellness Programming for companies & non-profits.
Inquire here, Wellness Catalog available: https://www.urbanhealthgroupllc.com/consulting-services.html
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-08964-3GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. DOI.CDC. (2018). Health United States, 2017. Table 46. Retrieved from https://www.cdc.gov/nchs/data/hus/hus17.pdf
CDC. (2019). Summary Health Statistics: National Health Interview Survey: 2017. Table A-7. Retrieved from https://www.cdc.gov/nchs/nhis/shs/tables.htm
CDC National Center for Health Statistics. Summary Health Statistics: National Health Interview Survey, 2018. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_P-11.pdf
Caplan S. (2019). Intersection of Cultural and Religious Beliefs About Mental Health: Latinos in the Faith-Based Setting. Hispanic health care international: the official journal of the National Association of Hispanic Nurses, 17(1), 4–10. https://doi.org/10.1177/1540415319828265
Jimenez, D. E., Bartels, S. J., Cardenas, V., & Alegría, M. (2013). Stigmatizing attitudes toward mental illness among racial/ethnic older adults in primary care. International journal of geriatric psychiatry, 28(10), 1061–1068. https://doi.org/10.1002/gps.3928. Accessed from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3672370/.
American Psychiatric Association. (2017). Mental health disparities: American Indians and Alaska Natives. https://www.psychiatry.org/File percent20Library/Psychiatrists/Cultural-Competency/Mental-Health-Disparities/Mental-Health-Facts-for-American-Indian-Alaska-Natives.pdf

